Skin Rash Misconceptions Debunked: Separating Fact from Fiction
Learn how skin rash misconceptions debunked can lead to improved diagnosis and treatment. Discover facts to navigate myths and ensure proper skin care.

Estimated reading time: 8 minutes
Key Takeaways
- Myths delay proper diagnosis and can lead to ineffective or harmful treatments.
- Not all rashes are allergic or contagious; causes vary widely.
- Natural remedies are not inherently safe and may contain hidden risks.
- Topical corticosteroids are effective and safe when used correctly.
- Persistent or unusual rashes require professional evaluation for accurate diagnosis.
Table of Contents
- The Roots of Skin Rash Misconceptions
- Common Skin Rash Myths and Why They’re Misleading
- Evidence-Based Insights on Skin Rashes
- Impact of Misbeliefs on Rash Diagnosis and Care
- Practical Tips for Evaluating and Managing Skin Rashes
- Conclusion
- FAQ
Section 1 – The Roots of Skin Rash Misconceptions
Outdated information lingers in medical circles and popular culture. Medicine advances, but old ideas die slowly. Patients and some clinicians still repeat decades-old advice—even when newer studies offer better guidance. This gap fuels many misconceptions, and debunking them begins by updating our beliefs about causes and cures.
Folklore and anecdotal remedies also spread myths through families and friends. When one person claims a home remedy cured their rash, others repeat it without proof. These tales can overshadow clinical evidence and lead to failed treatments or harm.
Misinformation online amplifies misunderstandings via unregulated health advice tied to products or paid ads. Commercial interests push unproven creams or secret formulas, and catchy posts often trump expert guidance. The result is persistent misconceptions that resist correction. Source: Debunking Dermatology Myths: Enhance Patient Care
Section 2 – Common Skin Rash Myths and Why They’re Misleading
Skin rash misconceptions often involve these five myths:
Myth 1: All rashes are allergic reactions
- Definition: An immune overreaction to an allergen like pollen, food, or chemicals.
- Reality: Rashes also arise from infections (bacterial, viral, fungal), autoimmune diseases (psoriasis, lupus), genetic factors (atopic dermatitis), or irritants (soaps, detergents, plants).
- Risk: Labeling every rash “allergy” delays proper testing and targeted care.
Myth 2: Skin rashes are always contagious
- Definition: A contagious rash spreads via touch or shared items.
- Reality: Many common rashes—eczema, psoriasis, and contact dermatitis from non-infectious irritants—are not contagious.
Myth 3: Natural remedies are always effective and safer
- Definition: Herbal creams, salves, and essential oils.
- Reality: Unregulated products may contain hidden corticosteroids; black salve can destroy healthy tissue.
- Risk: Hidden ingredients and poor quality control can cause burns, infections, or systemic harm.
Myth 4: Topical corticosteroids are dangerous and always cause harm
- Definition: Anti-inflammatory creams prescribed for diverse rashes.
- Reality: Under medical guidance, serious side effects like skin thinning are rare; proper dosing minimizes risks.
- Benefit: First-line therapy for many dermatoses.
Myth 5: All skin rashes are temporary and harmless
- Reality: Some rashes signal serious issues—systemic diseases like lupus or vasculitis, early skin cancer, or chronic inflammatory conditions needing long-term care.
- Advice: Persistent, changing, or painful rashes should prompt professional evaluation.
Section 3 – Evidence-Based Insights on Skin Rashes
Eczema Explained
Eczema is a chronic inflammatory disease marked by itchy, red, and cracked skin. It involves genetic and environmental triggers—stress, allergens, and seasonal changes. Understanding eczema’s root causes dispels the notion that it’s just a “dry skin” issue. Source: Debunking Eczema Myths
Effective Treatments Overview
- Topical corticosteroids remain first-line therapy, reducing inflammation and itching quickly.
- Non-steroidal options, like calcineurin inhibitors and biologics, offer long-term alternatives.
- Unproven “natural” therapies lack rigorous testing and may cause harm. Always consult a dermatologist first.
Expert Perspective
“Always see a dermatologist to get suspected skin cancer diagnosed properly and discuss treatment options if confirmed,” advises Dr. Smith, board-certified dermatologist. Early diagnosis ensures the right therapy and prevents complications. Source: Medical Myths: All About Skin
Section 4 – Impact of Misbeliefs on Rash Diagnosis and Care
Unchecked misconceptions can undermine patient care:
- Delayed or incorrect diagnosis when myths replace medical tests—patients may apply home remedies instead of seeking proper evaluation. Source: Debunking Dermatology Myths: Enhance Patient Care
- Steroid phobia leads to avoidance of effective topical corticosteroids, prolonging discomfort and risking secondary infections. Source: Debunking Dermatology Myths: Enhance Patient Care
- Harmful home remedies can cause burns or tissue damage, as seen with black salve and untested herbs. Source: Medical Myths: All About Skin
Consult healthcare professionals for unexplained, persistent, or severe rashes to ensure accurate diagnosis and safe, effective treatment.
Section 5 – Practical Tips for Evaluating and Managing Skin Rashes
Tip 1: Evaluate symptoms carefully
Note when the rash first appeared and how it has changed. Check for pain, fever, swelling, or blistering and record exposures like new soaps, plants, foods, or medications.
Tip 2: Be skeptical of online advice
Avoid decisions based on unverified testimonials. Seek peer-reviewed studies or reputable sources. Source: Debunking Dermatology Myths: Enhance Patient Care
Tip 3: Consult a dermatologist or healthcare provider
Seek evaluation if the rash worsens, spreads, accompanies fever or chills, or persists beyond two weeks despite home care. Virtual visits can be efficient; see our Online Dermatologist Consultation guide.
Tip 4: Avoid self-diagnosing with internet tools
Online quizzes and symptom checkers oversimplify complex conditions. Quality photos are essential for remote assessment; learn how with our tips for clear rash photos.
Always remember: expert assessment beats guesswork.
AI-Powered Preliminary Assessment
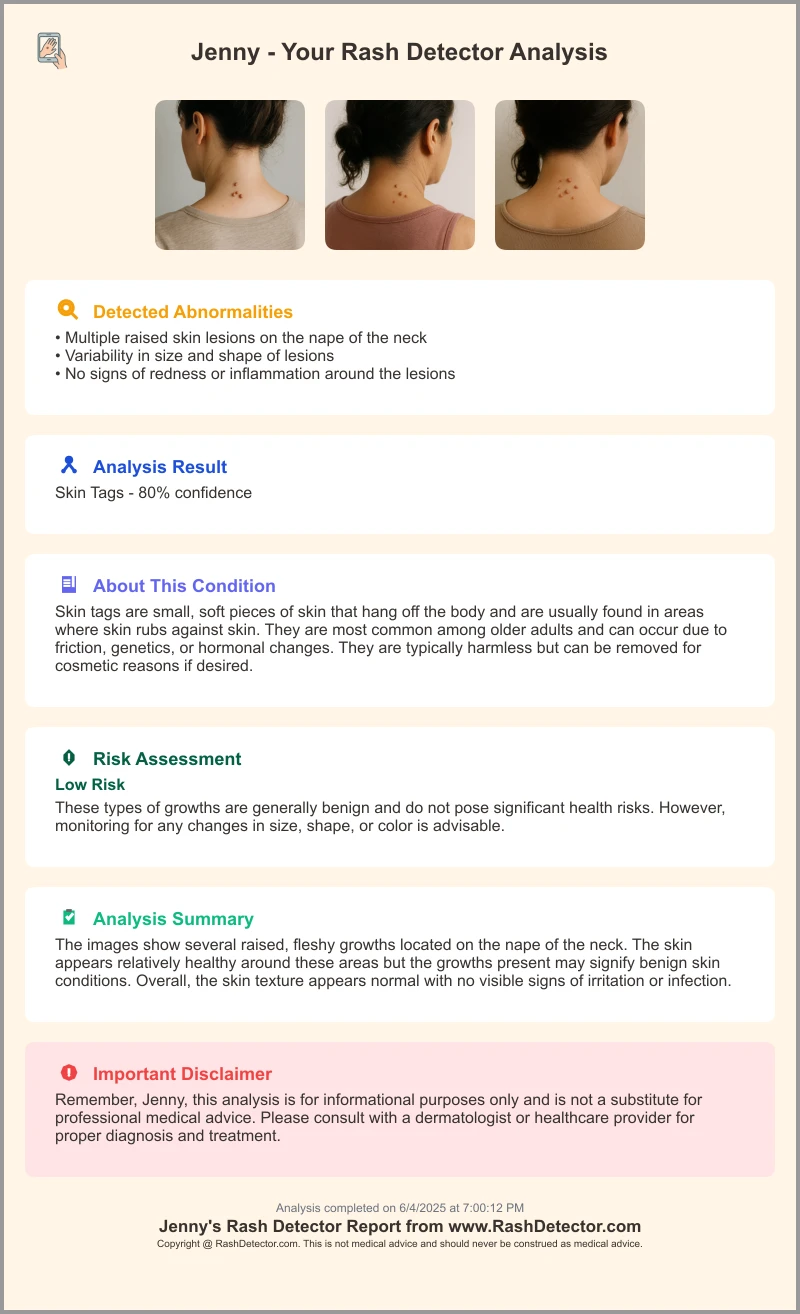
For a quick check, try the Rash Detector AI Skin Analysis App. Here’s a sample report:
Conclusion
Misinformation about skin rashes can lead to delayed diagnosis, improper treatment, and avoidable harm. By relying on evidence-based care, we dispel dangerous myths and improve patient outcomes. Share this post to help others move from confusion to clarity—accurate, safe, and effective rash management starts with evidence.
FAQ
Q: How can I tell if a rash is an allergic reaction?
A: Allergy rashes often appear suddenly, are itchy, and may be accompanied by swelling or hives. A dermatologist can confirm with a skin prick or patch test.
Q: Are natural remedies safe for treating rashes?
A: “Natural” does not guarantee safety. Unregulated products can contain hidden steroids or irritants. Always consult a healthcare professional before trying new remedies.
Q: When should I see a dermatologist for a rash?
A: Seek professional care if a rash worsens, spreads, is painful, accompanied by fever, or persists longer than two weeks despite home treatment.
Q: Can topical corticosteroids cause long-term harm?
A: Rarely, when used correctly under medical supervision. Proper dosing and treatment duration minimize risks like skin thinning or rebound flare.
Q: What are warning signs of a serious rash?
A: Look for persistent pain, rapid spreading, blisters, fever, or systemic symptoms. These require immediate medical evaluation.





