Understanding Vaginal Rash Causes and Prevention for Females
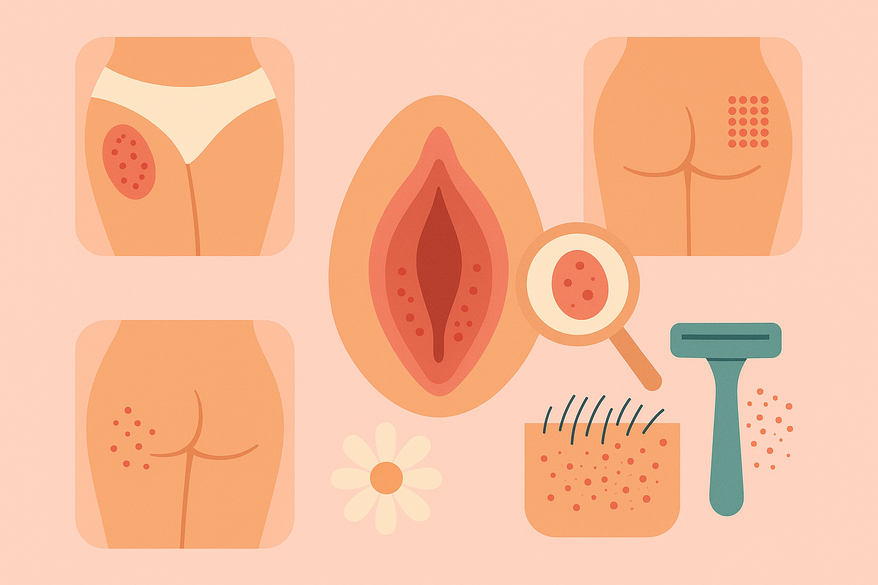
Explore causes of vaginal rash in females, with insights on jock itch vs heat rash, buttock rashes, and post-shaving irritation. Learn prevention tips for sensitive areas.
Estimated reading time: 8 minutes
Key Takeaways
- Vaginal rash basics: Irritation, redness, or bumps on the vulva often stem from dermatitis, infections, or friction.
- Jock itch vs. heat rash: Fungal rings versus sweat duct blockages—distinct triggers call for different self-care.
- Buttock rashes: Friction, moisture, and contact allergens are common culprits; hygiene and topical treatments help.
- Shaving irritation: Razor burn and ingrown hairs can be minimized with proper technique and soothing aftercare.
- Prevention: Hypoallergenic products, breathable fabrics, gentle cleansing, and lifestyle tweaks protect sensitive skin.
Table of Contents
- What Is a Vaginal Rash?
- Jock Itch vs Heat Rash: Key Differences
- Common Buttock Rashes in Adults & Treatment
- Managing Irritation After Shaving Your Pubic Area
- Overall Prevention and Skin Care Tips for Delicate Areas
What Is a Vaginal Rash?
Vaginal rash causes female discomfort through irritation, redness, burning, swelling, or bumps on the vulva. A rash here can range from mild pink patches to painful blisters. For more on general genital rash causes and when to worry, consider professional guidance.
- Contact Dermatitis
Allergic reactions to soaps, detergents, latex or fabrics. Symptoms include redness, itching, burning, and occasional blisters. - Infections
- Bacterial Vaginosis: Gray discharge, fishy odor.
- Yeast Infection: Thick white discharge, intense itch.
- Molluscum Contagiosum: Pearly, dome-shaped bumps.
- Scabies: Intense itch, tiny burrow lines.
- Other Irritants
Heat, moisture, and friction can cause chafing and inflammation.
Common symptoms: itching, burning, red or pink patches, swelling, or pain during intercourse or tampon use.
When to seek professional advice: severe or worsening itch; unusual discharge; sores lasting over a week despite OTC care; fever or spreading redness.
Jock Itch vs Heat Rash: Key Differences
jock itch vs heat rash can be confusing since both affect warm, moist areas like the groin and buttocks. Yet their causes and appearances differ:
- Jock Itch (Tinea cruris)
Fungal infection with ring-shaped, scaly red patches; very itchy and can spread. - Heat Rash (Miliaria)
Blocked sweat ducts produce clusters of tiny red bumps or blisters wherever sweat accumulates.
Key comparisons:
- Appearance: Jock itch has defined borders and scaling; heat rash shows uniform tiny bumps.
- Affected Areas: Jock itch targets inner thighs and groin folds; heat rash can appear under arms, back, and buttocks.
- Triggers: Jock itch thrives on fungal overgrowth; heat rash stems from sweat duct blockage in hot, humid conditions.
For a deeper dive on intertrigo and jock itch management between the legs, explore expert advice. If self-care (drying, antifungal powder) fails after 3–5 days, consult a provider for examination or culture.
Common Buttock Rashes in Adults
buttock rash adults often results from friction, moisture, or allergic contact. Redness, itching, and pain on the cheeks can disrupt daily life. Learn more about butt cheek rashes.
- Friction/Chafing: Tight clothing, repetitive movement, long sitting periods.
- Sweat & Moisture: Trapped sweat fosters bacterial and fungal growth.
- Contact Dermatitis: Irritation from soaps, detergents, fabric dyes, or toilet paper.
- Risk Factors: Obesity, sedentary habits, poor hygiene, excessive sweating.
Treating Rash Between Butt Cheeks
- Hygiene: Wash gently with mild, unscented soap; pat dry thoroughly.
- Topical Treatments: OTC hydrocortisone for inflammation; antifungal cream if needed.
- Clothing: Choose loose, breathable cotton or moisture-wicking underwear; skip tight synthetics.
- Monitoring: Watch for pus, pain, or fever—signs of infection.
- When to Consult: No improvement in one week or rash spreading beyond buttocks.
For AI-powered insights from photos, try Rash Detector:

Managing Irritation After Shaving Your Pubic Area
irritation after shaving pubic area can cause razor burn, micro-abrasions, and ingrown hairs. Adopting a careful approach prevents discomfort.
- Primary Causes: Dull blades, shaving against growth, fragranced products.
- Preventive Measures: Use a fresh razor on damp skin; apply fragrance-free shaving cream; shave with hair growth; rinse with cool water; pat dry and moisturize.
- Alternative Options: Trimming with scissors; waxing with proper aftercare; depilatory creams (patch-test first); professional laser reduction.
- Dermatologist Visit: Persistent redness or bumps beyond one week; signs of infection.
Overall Prevention and Skin Care Tips for Delicate Areas
Healthy habits and lifestyle tweaks can ward off many rashes in sensitive zones.
- Daily Habits: Use hypoallergenic, unscented soaps and detergents; wear breathable, moisture-wicking underwear; change wet clothes quickly; cleanse gently; keep skin folds dry.
- Lifestyle Adjustments: Maintain a healthy weight to reduce friction; shower after heavy sweating; opt for loose clothing in heat.
- When to Escalate Care: Rashes lasting over a week; worsening or spreading; systemic signs like fever or swollen lymph nodes.
FAQ
Q: How do I know when to see a doctor for a vaginal rash?
A: If itching worsens, discharge is unusual or painful, sores last beyond one week, or you experience fever or spreading redness, seek professional care.
Q: Can I treat jock itch and heat rash with the same remedies?
A: No. Jock itch requires antifungal approaches, while heat rash improves with cooling, drying, and barrier creams. Evaluate your symptoms before choosing treatment.
Q: What’s the best way to prevent razor burn in the pubic area?
A: Use a sharp blade, shave on damp skin with fragrance-free cream, follow hair growth direction, rinse with cool water, and apply a soothing moisturizer or aloe vera.
Q: Are there home remedies for buttock rashes?
A: Gentle cleansing, keeping the area dry, loose breathable clothing, and OTC hydrocortisone or antifungal creams can help. Consult a provider if symptoms persist.





