Evaluating the Cost Effectiveness of Rash Diagnosis Apps
Explore the cost effectiveness of rash diagnosis apps, their pricing models, savings, and ROI insights to understand how they reshape dermatology workflows.

Estimated reading time: 8 minutes
Key Takeaways
- Rash diagnosis apps offer rapid, at-home triage, reducing wait times from days to minutes.
- These tools can save 30–40% on typical visit costs, with subscription and freemium models suiting different users.
- Accuracy ranges around 80–90% for common rashes, complementing rather than replacing professional exams.
- Institutions can realize annual savings of $50K or more by diverting routine cases through apps.
- Future trends include deeper AI integration, telehealth workflows, and insurance reimbursement for digital screenings.
Table of Contents
- Introduction
- Market Overview of Rash Diagnosis Apps
- Understanding Cost Effectiveness
- Pricing and Subscription Models
- Comparative Analysis vs Traditional Care
- Commercial Considerations
- Future Trends and Innovations
- Conclusion
Introduction
The cost effectiveness of rash diagnosis apps is transforming how patients and providers approach skin care. These mobile or web platforms use AI, symptom checkers, or image databases to provide preliminary assessments of skin rashes. By uploading photos or entering symptoms, users receive possible condition matches and next-step guidance within minutes.
Cost effectiveness matters because it determines:
- Affordability for individuals seeking at-home triage
- Resource optimization for healthcare systems under budget constraints
- Faster intervention to prevent complications and downstream expenses
In this post, we cover market overview, key cost-effectiveness criteria, pricing models, comparative analysis vs traditional care, commercial considerations, future trends, and actionable recommendations.
Market Overview of Rash Diagnosis Apps
Rash diagnosis apps function as digital triage tools. Users either photograph their rash or input symptoms. The app’s AI returns possible diagnoses (e.g., eczema, psoriasis), risk levels (urgent vs non-urgent), and next-step recommendations (self-care tips or seek professional care), enabling early detection and timely medical attention.
Key growth drivers:
- Rising global prevalence of skin disorders
- Heightened consumer health awareness
- Advancements in AI, computer vision, and cloud computing
Projected market size: Disease management apps are set to grow from $11.55 billion in 2024 to $13.11 billion in 2025. User segments include individual consumers, telehealth providers, and insurers seeking cost containment via remote screening.
Sources: Disease Management Apps Market Report, Skin Rash Treatment Market Report
Understanding Cost Effectiveness
Cost effectiveness in healthcare measures clinical benefits relative to monetary cost. For rash diagnosis apps, focus on technical accuracy, reduced time to diagnose, and potential savings.
A. Technical Accuracy
- Metrics: sensitivity, specificity, positive predictive value
- Example: Aysa app from VisualDX uses deep learning and a large image database, reporting high sensitivity and instant feedback.
- Impact: Greater diagnostic confidence reduces false reassurance and unnecessary visits.
Source: VisualDX Blog
B. Reduced Time to Diagnose
- Traditional wait: Average dermatology appointment can take up to 32 days.
- App analysis: Immediate results in minutes via AI triage engine.
- Benefit: Faster triage prevents escalation and cuts downstream treatment costs.
C. Potential Savings
- In-person visit cost: Typically > $100 (visit fee, facility charge).
- App visit cost: Often < $20 for a diagnostic session or subscription access.
- System savings:
- Fewer non-urgent visits free up specialist capacity
- Lower insurer payouts on routine cases
- Reduced patient travel and lost-work costs
Leveraging apps for benign rash screening can yield 30–40% cost savings per case.
Pricing and Subscription Models
Apps adopt three main pricing structures, each influencing overall cost effectiveness.
Model A: One-Time Purchase
Single upfront fee for permanent access to core features.
- Pros: No recurring charges; predictable cost for infrequent users.
- Cons: Updates may require paid upgrades; may lack ongoing AI improvements.
- Value vs Traditional Visit: $50–$100 one-time vs $100+ per in-person appointment.
Model B: Freemium
Free basic screening; premium diagnostics or tele-dermatology consults at extra cost.
- Pros: Low barrier to entry; drives trials.
- Cons: Critical features paywalled; potential hidden costs.
- Value vs Traditional Visit: Core screening free or <$5 per use; premium consults $15–$30 vs $100+ co-pay.
Compare features: free vs paid rash detector
Model C: Subscription (Monthly/Annual)
Recurring fee unlocks full feature set, updates, expert consultations, and telehealth integration.
- Pros: Continuous updates; budget predictability for institutions.
- Cons: Costs accumulate for low-usage consumers; commitment periods may apply.
- Value vs Traditional Visit: $10–$20/month for unlimited sessions vs one dermatology co-pay.
Hidden Costs to Highlight
- In-app purchases for specialist reports or follow-up scans
- Data-usage fees for high-resolution uploads
- Insurance co-pays if telehealth consults are billed separately
Comparative Analysis vs Traditional Care
| Metric | App | In-Person |
|---|---|---|
| Upfront Cost | <$20/session or subscription | >$100/visit |
| Time to Result | Minutes | Days–weeks |
| Accessibility | 24/7 remote access | Scheduled visits |
| Diagnostic Accuracy | ~80–90% for common rashes | Higher for complex cases |
| Follow-Up | Automated reminders, telehealth booking | Manual scheduling, extra fees |
Case Study: Aysa’s AI-driven triage reduced non-urgent clinic traffic by ~35%, saving 30% on routine visit costs. Diverting 1,000 benign rash visits at $100 each to $20 app visits can save roughly $80,000 annually.
Commercial Considerations
For Consumers
- Apps often cost less per use than insurance co-pays.
- Convenience savings: no travel, less time off work.
- Decision factors: accuracy ratings, pricing structure, expert consult availability.
For Healthcare Institutions
ROI potential:
- Average saving per diverted case: $50
- Cases triaged per year: 1,000
- Annual saving: $50 × 1,000 = $50,000
Barriers to adoption include data privacy, EHR integration, and workflow alignment.
Future Trends and Innovations
- AI Advancements: Deep learning refinements, expanded condition libraries, real-time updates.
- Integrated Telehealth: End-to-end workflows: upload → AI triage → video consult → e-prescribing.
- Market Shifts: Enhanced freemium models, bundled services, insurance reimbursement for digital screeners.
Conclusion
Rash diagnosis apps deliver prompt, affordable screening, reducing costs and wait times compared to traditional care. By understanding one-time, freemium, and subscription models—and accounting for hidden fees—users and institutions can choose the best value.
- Analyze usage to select the optimal pricing structure.
- Leverage apps for initial triage; consult professionals for complex cases.
Actionable Advice:
- Compare subscription vs one-time fees based on rash-assessment frequency.
- Verify included expert consult options and insurance compatibility.
- Download trial versions or request demos to test accuracy and workflow integration.
For a deep dive into cost-effective solutions, check out affordable AI skin diagnosis.
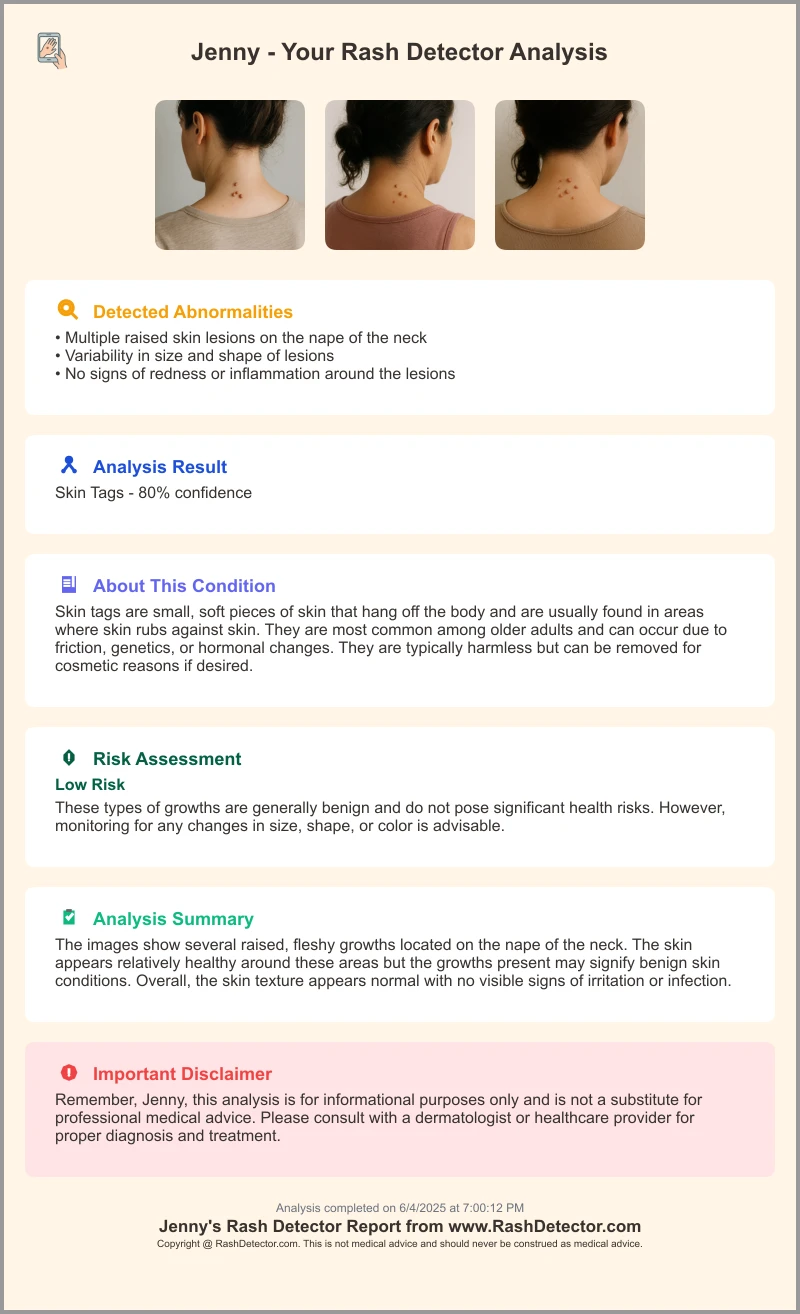
Try the Rash Detector to upload images and receive an AI-driven assessment report in minutes.
FAQ
-
Q: How accurate are rash diagnosis apps?
A: Most apps achieve around 80–90% accuracy for common rashes but should complement professional evaluation for complex cases. -
Q: What cost savings can I expect?
A: Users can save 30–40% per case compared to in-person visits; institutions may save over $50,000 annually by diverting routine screenings. -
Q: Which pricing model is best?
A: Infrequent users benefit from one-time purchases; regular users or institutions often prefer subscriptions for predictable costs and updates. -
Q: Are my personal images secure?
A: Reputable apps use encryption and comply with data privacy regulations; always review the privacy policy before uploading sensitive images. -
Q: Can these apps replace dermatologists?
A: No; they are designed for initial triage and screening. Complex or urgent cases require professional consultation.





