Understanding Rash in Rheumatoid Arthritis: Causes, Types & Management
Explore the causes, types, and management of rash in rheumatoid arthritis, a complex systemic condition affecting skin and joints. Learn about diagnosis and treatment.

Estimated reading time: 10 minutes
Key Takeaways
- RA is systemic: It can manifest in the skin as well as joints.
- Multiple causes: Flares, vasculitis, medications or direct autoimmune attack.
- Varied rash types: From vasculitic ulcers to palmar erythema.
- Diagnosis: Clinical exam, biopsy and laboratory tests guide care.
- Treatment: Topical steroids, systemic DMARD adjustments, antibiotics and lifestyle measures.
- Prevention: Vigilant skin care, medication monitoring and early action minimize complications.
Table of Contents
- Understanding Rheumatoid Arthritis
- Exploring Skin Manifestations in RA
- What Causes a Rash in Rheumatoid Arthritis?
- Types of Rashes Associated with RA
- Diagnosis and When to Seek Medical Advice
- Management and Treatment Options
- Impact on Quality of Life
- Practical Advice and Prevention Strategies
- Conclusion
Understanding Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a chronic, systemic autoimmune disorder targeting the synovial lining of joints. Beyond joint pain, swelling and stiffness, RA can involve lungs, eyes, skin and blood vessels.
Common systemic symptoms include:
- Persistent joint pain and stiffness
- Fatigue, loss of appetite
- Fever and malaise during flares
Inflammatory cytokines released in RA can travel to the skin, paving the way for a autoimmune skin manifestations.
References: Cleveland Clinic, Physio-Pedia
Exploring Skin Manifestations in RA
Skin involvement in RA arises when systemic inflammation extends beyond joints. Patients may develop:
- Rashes or red plaques
- Firm subcutaneous nodules
- Ulcers or nonhealing sores
- Red, irritated patches
Such changes can indicate active disease, a flare marker or a reaction to RA therapy.
References: Healthline, HealthCentral
What Causes a Rash in Rheumatoid Arthritis?
Skin changes in RA can stem from several mechanisms:
- Active RA flares: High cytokine levels reduce skin blood flow, causing red or purple rashes and ulcers.
- Rheumatoid vasculitis: Immune complexes inflame vessel walls, leading to red patches or ulcers, often on the legs.
- Medication effects: DMARDs and biologics may trigger allergic rashes or lower immunity, resulting in infections.
- Direct autoimmune attack: Skin cells become targets, forming plaques or lesions with immune cell infiltration.
In summary, RA-associated rashes can result from disease activity, vascular inflammation, drug reactions or direct immune damage.
References: HealthCentral, Healthline
Types of Rashes Associated with RA
- Rheumatoid Vasculitis Rash
Red, inflamed patches or ulcers on lower legs; symmetrical and painful; requires prompt care. - Interstitial Granulomatous Dermatitis
Red or purple bumps and plaques on trunk and limbs; microscopically shows granulomas. - Palmar Erythema
Diffuse redness of the palms extending to fingers; common and non-itchy. - Rheumatoid Nodules
Firm, round subcutaneous bumps on elbows or hands; more a skin change than a rash.
Diagnosis and When to Seek Medical Advice
Evaluating an RA rash includes:
- Reviewing RA history and treatments
- Skin exam: shape, color, symmetry
- Skin biopsy for vasculitis or granulomas
- Blood tests: ANA, RF, ESR, CRP
- Excluding infections and drug allergies
Seek urgent care if the rash:
- Spreads rapidly or becomes painful
- Shows infection signs (pus, fever)
- Develops open ulcers
- Accompanies systemic symptoms (weight loss, night sweats)
References: Healthline, WeDerm
Management and Treatment Options
Therapy depends on the rash’s cause:
- Topical therapies: Medium-strength corticosteroid creams for local inflammation.
- Systemic adjustments: Optimize DMARDs or short oral steroids for vasculitis.
- Antibiotics/antifungals: For immunosuppression-related infections; guided by cultures.
- Skin care: Gentle cleansers, daily moisturizers, soft fabrics, sun protection.
- Complementary: Oatmeal baths for itch relief; stress reduction to lower flare risk.
Emerging studies show tighter RA control often reduces rash severity and frequency.
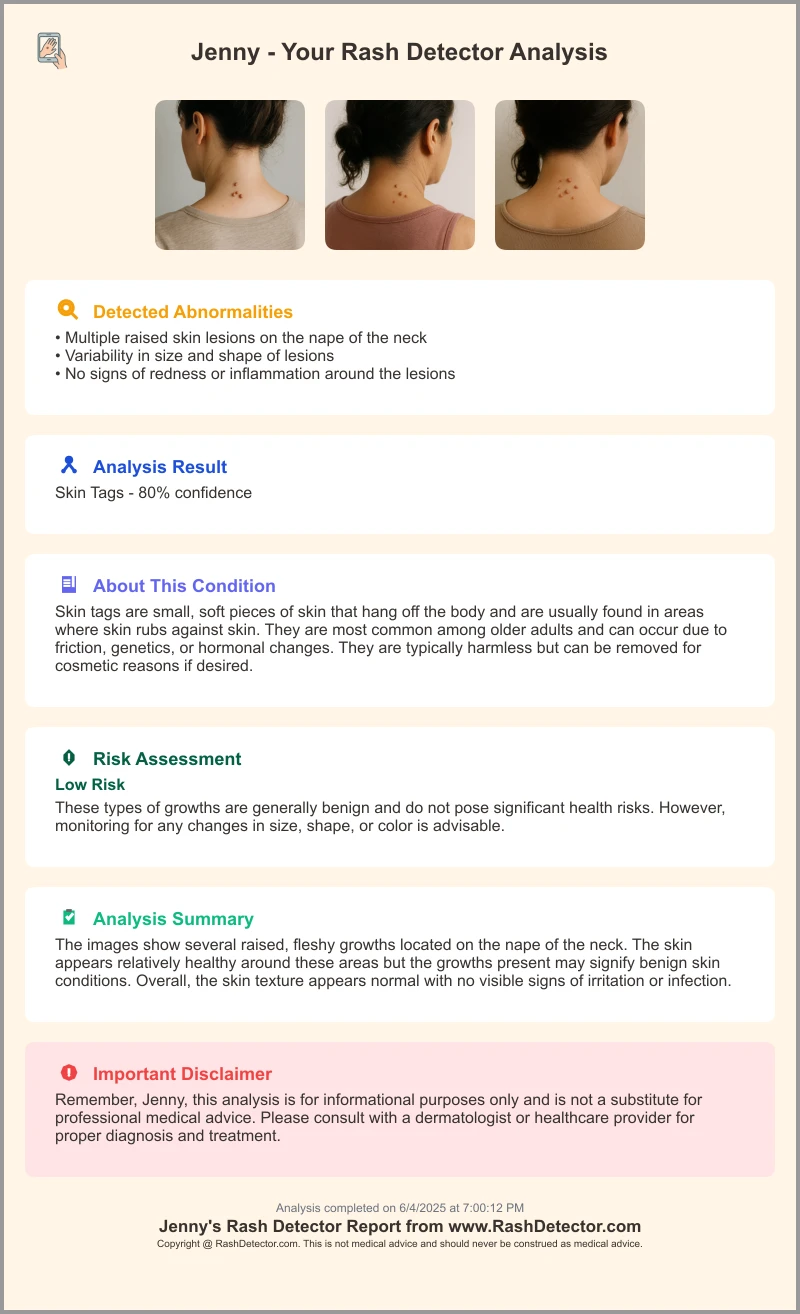
For digital tracking and instant feedback, patients can use the Skin Analysis App. Upload photos and receive a quick report.
Impact on Quality of Life
RA rashes can affect daily living:
- Physical discomfort: Itching, burning or pain limiting hand use or walking.
- Cosmetic concerns: Visible changes may cause self-consciousness or social withdrawal.
- Emotional effects: Anxiety over flare-ups; depression from chronic appearance issues.
Support strategies: Join patient communities, seek counseling and share coping tips with your care team.
Practical Advice and Prevention Strategies
- Self-monitoring: Photograph new rashes, note date, location and related RA activity.
- Skin care routine: Use mild, sulfate-free soaps and fragrance-free moisturizers twice daily; wear sunscreen.
- Medication vigilance: Keep an updated list of RA drugs; report new rashes to your rheumatologist.
- Early signs: Symmetrical redness, persistent itching or any skin break.
Prompt action often prevents minor rashes from worsening.
Conclusion
Rheumatoid arthritis is a systemic condition that may present with diverse skin rashes—from vasculitis to palmar erythema. Early recognition, accurate diagnosis and tailored management—whether topical treatments, systemic adjustments or lifestyle measures—are key to controlling skin symptoms. Collaborate with your rheumatologist and dermatologist, and seek care promptly for new or worsening skin changes.
Additional Resources
• Arthritis Foundation
• National Psoriasis Foundation
• CreakyJoints patient community
• Vasculitis Foundation
FAQ
- What are common skin manifestations of RA?
- They range from vasculitic ulcers and red plaques to palmar erythema and nodules.
- How is an RA-related rash diagnosed?
- Through clinical history, detailed skin exam, biopsy, and laboratory tests (ANA, RF, ESR, CRP).
- When should I see a doctor for an RA rash?
- If the rash spreads rapidly, becomes painful, shows infection signs, or accompanies systemic symptoms.
- Can medication changes prevent RA rashes?
- Yes. Adjusting DMARDs or biologics under medical supervision can reduce rash risk.
- Are RA rashes reversible?
- With early intervention and proper treatment, many rashes improve or resolve completely.





